Can I get Pregnant with a Spinal Cord Injury?
A common misconception repeatedly revealed in medical literature is that many women with spinal cord injuries assume that if they’re legs are not moving, nothing below their waist is “working” which is not the case. Having a SCI does not prevent a woman from becoming naturally pregnant, carrying or delivering a baby. In fact, a recent article from the journal Spinal Cord Injury and Cases tells us that pregnancy is relatively safe in women with spinal cord injuries and that women with SCI’s remain fertile and have equal chance of pregnancy.
In addition, medical technology and modern pharmaceuticals are helping spinal cord injury victims recover better, and live fuller and complete lives. A 2016 study in the medical journal Spinal Cord, noted that there have been major improvements in the overall health outcomes for persons with spinal cord injury (SCI) over the last half century – and growing recognition that spinal cord injury victims can live full and rich lives . Becoming pregnant has been increasingly accepted and a successful option for women with spinal cord injuries.
A common question during the stages of change and rediscovery
Spinal cord injuries can happen to anyone-young or old, male or female, of any race, religion, or socioeconomic status. They are often caused by motor vehicle or diving accidents, but they can also result from medical conditions such as tumors or infections, gunshot wounds, falls, or freak accidents. Recovery after a spinal cord injury is a long process physically, mentally, and emotionally.
From what our personal injury lawyers see with our clients, it seems that there is nothing really predictable about the psychological sequelae of SCI. Every person handles the psychological impact of a spinal cord injury differently, dependent on such things like whether or not they suffer an accompanying head injury (research shows that up to 50% of SCI victims suffer head injuries in traumatic accidents) their pre-accident personality, their predisposition to depression and anxiety how they handles stages of grief and their overall acceptance of the injury. One thing is common however – for people who experience spinal cord injuries between the ages of eighteen and their mid-thirties, the prime years for childbearing, fertility – the ability to have children is often a major concern to them.
Pregnancy and Spinal Cord Injury
The American College of OBGYN’s have an excellent spinal cord injury resource centre regarding pregnancy and spinal cord injuries. The ACOBGYM states that being paralyzed does not usually change a persons “desire” to become a parent and for women, they should not be deterred from the idea of pregnancy and parenthood after SCI. For a mother-to-be who receives the appropriate monitoring from an obstetrician familiar with her particular situation, paralysis should have little impact on pregnancy, labor, and delivery. Although though there may be some roadblocks along the way, many women have shown that, with commitment and adaptability, successful pregnancies are indeed possible (and increasingly common).
This article is written primarily for women who want to gain a better understanding of the impact of pregnancy with an SCI. Although post-injury pregnancies do carry a risk for more complications, outcomes for both mothers and their infants are excellent, provided that the moms are in good general health and receive close monitoring. In this article, we discuss, with the appropriate research, how important it is to find the right health care provider as most family doctors are unfamiliar with pregnancy and spinal cord injuries, as well as some common side effects and complications that a woman with a spinal cord injury may experience while pregnant.
Finding a Health Provider
The ACOBGYN’s tells us that one of the greatest initial obstacles to motherhood is finding healthcare care professionals experienced in the management of pregnancy as well as labor and delivery in women with SCI. While the odd general practitioner may have experience treating women with serious disabilities, it is highly unlikely that your GP has treated a woman with a spinal cord injury throughout her pregnancy. In fact, we have been told by our experts that pregnancy and SCI issues are typically not a part of medical school curriculums.
Once a woman finds a competent doctor who is comfortable with the situation, she should be reassured that pregnancy is indeed possible-and that more and more paralyzed women are conceiving, carrying their babies to term, and having normal spontaneous vaginal deliveries. It may require some work to find health care providers who have experience in this area, or you and your occupational therapist may in fact need to educate your health care provider about some of your unique needs.
A Multidisciplinary Approach
The American College of OBGYN’s actually recommends that pregnancy in women with SCIs should be managed not just by a family doctor and OBGYN but rather “by a multidisciplinary team approach involving specialists, which may include an obstetrician with experience in caring for women with disabilities, maternal-fetal medicine subspecialists, anesthesiologists, spinal rehabilitation physicians, nurses, physiotherapists, occupational therapists, lactation consultants, pediatricians, and neonatologists.” Building a pregnancy team can be a good way of optimizing your care. If you can’t find team members who have experience working with people with SCI, then having doctors and therapists who are interested in learning the issues is critical.
You have several options when choosing a health care provider for pregnancy care.
An obstetrician/gynecologist gynecologist (often referred to as “OB/Gyn”) is a doctor who specializes in the medical and surgical care of women during pregnancy, childbirth, and after delivery. This type of physician has the most training in pregnancy and childbirth issues.
A perinatologist is an OB/Gyn who specializes in the care of the mother and the fetus, who may have a higher chance of complications.
Other professionals offer services to women, such as certified nurse mid-wives (CNM) and doulas. A CNM is a specially trained registered nurse, who has experience in providing obstetric and newborn care. Midwives work with obstetricians, who are available to assist if complications occur during pregnancy, labor or delivery.
A doula is a person who specializes in helping families through the childbearing childbearing year. Because they do not provide any clinical care, you still need to choose an obstetric health care provider since the services of a doula are typically not covered by insurance benefits.
Pubmed research tells us that pregnant women with SCI can certainly be at risk for certain complications. For this reason, in most cases it is probably best that you choose an obstetrician or perinatologist who has experience treating women with SCI. In some cases a general or family practitioner may be amply qualified to take care of your obstetric needs, especially if that person has experience working with others with SCI and if you have a mild injury and are not at risk for many complications (such as autonomic dysreflexia).
When choosing a primary obstetric health care provider, you need to weigh the following factors:
- Do you prefer an OB or are you comfortable with a qualified generalist or midwife?
- If you prefer an OB, would you feel more comfortable with a perinatologist?
- What priority do you put on your health care provider having experience treating other women with SCI?
- How far away is you health care provider?
Common Pregnancy Side Effects
Dr. Amy Jackson of the University of Illinois did a comprehensive study a few years back comparing women who had been pregnant both before and after a SCI. The study found that complications such as morning sickness, anemia, toxemia, and vaginal bleeding did not change between “before” and “after” groups. In other words, SCI did not affect many of the “common”pregnancy symptoms. [mini_cta id=”24″ align=”left”]
In reviewing A Disabled Women’s Guide to Pregnancy and Birth the author reports on a survey about problems encountered during pregnancy of women with SCI. She found that the most common first trimester complaint was nausea, followed by fatigue and leg spasms. In the second trimester, leg spasms were the most common followed by impaired mobility and transfers, urinary tract infection, and edema (swelling of the feet and lower legs). In the third trimester, impaired mobility and transfers, edema, back pain, and spasms were the major problems reported.
Other complaints reported consistently, but to a lesser degree, included constipation, heartburn, other urinary problems, and breathing issues. Of 16 pregnancies in women with SCI T6 and higher, 4 reported autonomic dysreflexia in the third trimester. Most of these complaints seem to be common complaints of all women who are pregnant. Some secondary complications of SCI are also typical of pregnancy and are likely to be exacerbated by pregnancy. Therefore, many of the problems are not new, but because of your SCI, a woman may find additional ways to deal with these old problems.
Some common problems experienced by women with SCI’s during pregnancy:
Weight Gain – although weight gain during pregnancy is a reality for all women, those who use wheelchairs have an even greater likelihood of adding extra pounds. Their increased girth may also worsen the indigestion and heartburn typically experienced by expectant mothers as the growing uterus presses up on the stomach and irritating digestive fluid backs up into the esophagus. Moreover, women with cervical or high thoracic injuries may find that their larger size and expanding uterus affect their ability to breathe easily, though in most cases proper positioning and adequate rest are usually enough to prevent serious problems like pneumonia. monia. For those with chronic pain, additional pounds may increase crease the overall load on skeletal joints, adding to discomfort and making transfers and positioning more difficult.
Fatigue – is very common in women during pregnancy. The obvious way to handle fatigue is to rest when you feel the need, but this solution is often easier said than done.
Spasticity – because several of the medications used to treat spasticity in paralyzed individuals can pose risks to a developing fetus, physicians will usually taper and stop these drugs during pregnancy, which would increase muscle tone. Spasticity can be increased because of the pregnancy – but Dr. Jackson tells us it can be a symptom of another problem such as bladder infection, or it can even be the first symptom of labor. Therefore, it’s important for you to monitor your spasticity carefully and consider what else might be causing a change in spasticity.
Constipation – all pregnant women are prone to constipation during pregnancy, but constipation can be more of a problem for women with SCI. After a SCI it takes longer for your intestinal muscles to push stool through your gastrointestinal tract, putting you at greater risk of constipation. Pregnancy also causes constipation because your growing uterus puts pressure on your rectum making it more difficult for stool to pass.
Urinary Problems and Bladder Infections – as the uterus grows, a pregnant woman with spinal cord injury may experience increased difficulty in fully emptying her bladder. As a result, urinary tract infections are often the most common complication during pregnancy. Some women also note increased creased urine leakage, which is best treated by catheterizing more often or switching to indwelling catheters, though both options tend to heighten the chance for infections.
In additions, self-catheterization can be much more difficult during pregnancy because your pregnant belly blocks your vision. Because of other issues with intermittent catheterization, some women with spinal cord injuries have reported having to switch to an indwelling catheter during pregnancy. Other concerns with indwelling catheter use is that the bladder may lose its elasticity, or ability to stretch and hold larger amounts of urine, or the catheter may slip out of the urethra, perhaps because of either frequent bladder spasms and/or the baby pushing on the bladder.
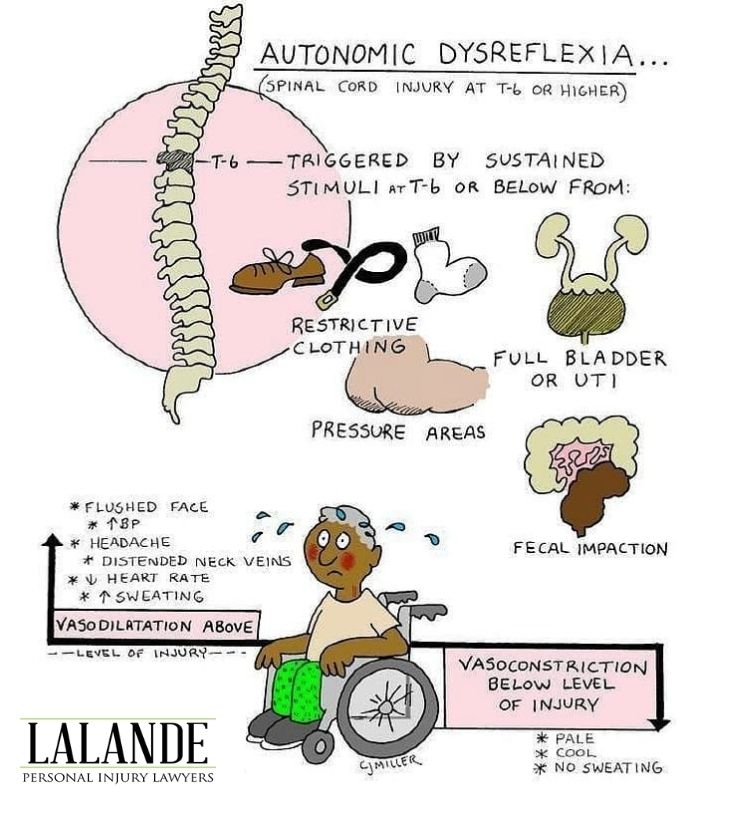
Autonomic dysreflexia – is a spinal cord injury-specific problem that can occur during pregnancy for a variety of reasons. The American College of OBGYN’s tells us that from their perspective, autonomic dysreflexia (sometimes called autonomic hyperreflexia) is the most serious medical complication that occurs in women with SCIs and is found in 85% of patients with lesions at or above T6 level. It is a life-threatning complication of SCI’s and most likely to arise during labor.
This condition is a reaction of the autonomic (involuntary) nervous system to certain irritating stimulation. Autonomic dysreflexia causes an imbalanced reflex sympathetic discharge, leading to potentially life-threatening hypertension. It is considered a medical emergency and must be recognized immediately. Symptoms include high blood pressure, change in heart rate, skin color changes (pallor, redness, blue-gray coloration), and profuse sweating. During pregnancy, you may experience autonomic dysreflexia caused by a bladder infection, bladder distention (from increased extra fluid intake), increased fluid from the baby, excessive pressure on the skin, or other common causes of dysreflexia.
Because autonomic dysreflexia is most likely to occur during labor, delivery is recommended at a “Group A” Ontario hospital, when possible, for a patient with SCI.
R.N. CJ Miller, a well known medical artist, provided the following understanding of autonomic dysreflexia:
Breathing Problems -many women experience pulmonary, or breathing, changes during pregnancy because a pregnant woman’s expanding belly takes up some of the room in her abdomen, limiting the amount her lungs can expand. It is also because of the extra energy demands of pregnancy. Additionally, if you have a high thoracic or cervical spinal cord injury, your lung function is limited as well.
Blood Clots – all women have an increased tendency to develop blood clots during pregnancy; for those with SCI, decreased mobility further ther adds to the risk. These clots (blockages known as deep venous nous thromboses) usually form in the veins of legs but can also travel to the lungs (as pulmonary embolisms), which can be life-threatening. threatening. All paralyzed individuals and their families need to be aware that any increased warmth, redness, or swelling in a leg can indicate the presence of a blood clot. If such a clot extends tends to the lungs, shortness of breath or chest pain can occur suddenly. And if these symptoms are noted, immediate medical attention is necessary.
Pressure Sores: although the risk of “skin pressure” increases during pregnancy, a study by Dr. Jackson found that, suprisingly, one study found that only 6 percent of pregnant women with spinal cord injury experienced a pressure sore. In nearly all cases, a pressure sore is a preventable complication of spinal cord injury. Whether you are pregnant or not, it is important to continue to perform your twice daily skin checks, eat a healthy diet, drink a healthy amount of water, and do your weight shifts every 15 minutes to 20 minutes. Additional considerations during pregnancy include using a larger wheelchair to accommodate your growing body (described in greater detail below) and suggesting that your doctor incorporate skin checks into your regular doctor appointments.
Labour Pains and Delivery – in the medical journal entitled The impact of spinal cord injury on female sexuality, menstruation and pregnancy: a review of the literature Dr. Sipski tells us that the more serious problem with pregnancy and SCI is management of labor, especially if the woman cannot perceive labor pains or contractions. Therefore, if the level of lesion is at T10 or higher, there is a possibility you may not know you are in labor – you probably will not feel labour pains. It is important that you closely monitor your bodily responses and schedule weekly visits to your obstetrician by the time you are into your third trimester month of pregnancy.
An article in Paraplegia, entitled Pregnancy, labor and delivery post spinal cord injury tells us that most women with Spinal Cord Injuries can deliver vaginally unless they suffer from gynecological problems that are unrelated to your spinal cord injury. In addition, BMC Pregnancy and Childbirth tells us that current evidence supports the notion that pregnancy outcomes are generally successful and that vaginal delivery can be safely achieved in the majority of women, independent of the level of Spinal Cord Injury.
Also with loss of sensation, delivery may be quicker compared to a woman without a spinal cord injury due to the loss of sensation and muscle tone changes that occur after a spinal cord injury. The alternative to vaginal delivery is cesarean section or C-section. This surgery involves delivery of the baby through an incision near the mother’s pubic line, rather than through the birth canal. C-section can be a life-saving surgery if you have autonomic dysreflexia that is not improving with medications or anesthesia.
Breastfeeeding with a Spinal Cord Injury – There are several medical journals which indicate that breastfeeding is encouraged even in women with high cervical lesions/ injury. Many articles, however, support the notion that spinal cord injury (particularly at or above T6) disrupts lactation and is associated with shorter breastfeeding duration. There are several challenges to take into account in regards to breastfeeding which are unique to spinal cord injury. These challenges include low milk production, autonomic dysreflexia, spasticity, breast infection, and positioning the baby.
Spinal Cord Injuries which Occur During Pregnancy
Believe it or not, spinal cord injuries occurring during pregnancy is very rarely reported. However, the journal Spinal Cord Cases tells us that pregnancies in women with spinal cord injury are at greater risk of morbidity and mortality. The burden of care of a pregnant woman who suffers a spinal cord injury increases dramatically because of abrupt and traumatic changes to body physiology. The resulting spinal cord disability as extreme risk and stress to fetal well being.
In particular, this article discusses the case of a young lady who suffered a traumatic spinal cord injury at the C6 level during her second trimester of pregnancy. The article emphasized that multisystem involvement due to spinal cord injury during pregnancy does result in intense physiological changes which can cause indirect or direct fetal injury or death. Causes of fetal fatality during spinal cord injury were noted to be spontaneous abortion, marked disability or malformation, prematurity and premature labour especially with women who suffered upper thoracic and cervical spinal cord injury. Other causes of fetal injury and death were noted to be major and blunt trauma to the abdomen.
Before reading this article it is important to understand that under any circumstances we are not providing medical advice. We are not doctors. We work with doctors everyday on our cases and are lucky to be guided, gain knowledge and be educated by the best doctors about medical issues that we routinely deal with. If you or a loved one suffers from a spinal cord injury and has a pregnancy related question, please speak to your GP, OBGYN or physiatrist. This article was written as an information piece only. This article was written in consultation with Dr. Amy Jackson, a physiatrist who specializes in SCI and Childbirth.
Other things to Consider
In speaking with our experts, in particular certified life care planners, there are other things to consider. For example, you may require a custom built crib with an opening that best suits your ability to access your baby. There are also portable cribs on the market on rollers which would allow easier access. You may also require extra breast-feeding pillows to assist in positioning of your baby. At times, you may need properly placed breast-feeding pillows in order to counteract the lack of strength or mobility. An occupational therapist will be able to assist you with this.
You may also require a functional area to be set up in your home so that you can safely change your baby’s diapers. In one case, we assisted with the construction of a table with open sides and a safety belt for the baby, that sat just at the right height for our client to sit and care for their child.
Another issue to consider is pushing your wheelchair with your baby. We have learned that there are baby slings to assist spinal cord injury victims carry their babies well in their wheelchair. When the infant is then old enough to set up, you can purchase infant harnesses and a strap your baby onto your lap for safety transport when you are moving your wheelchair. Also, there are harnesses available to ensure your child’s safety when he or she starts walking. If you are outside, these harnesses would save you the frustration or fear of your child dashing into the roadway or away from your attention.
It’s very important that you keep the communication lines open with your therapist, occupational therapists, rehab nurses etc. to help provide you with adaptive training for feeding, dressing, changing, bathing in transporting your baby.
Get the Justice you Deserve
If you or a loved one has suffered a spinal cord injury because somebody else was careless, it is important that you contact a qualified personal injury lawyer with expertise in spinal cord injuries sooner rather than later. We always recommend that it’s best to contact a qualified spinal cord injury lawyer prior to hospital discharge. It’s important that insurance funding is put into palce, that issues are dealt with, that the insurers involved know that you have retained an advocate, and that the proper occupational therapists who know and who have worked with your lawyer assist you with your discharge and transition home. Lots needs to be put into place. In addition, it’s important to commence your life care plan development within the context of all your future rehabilitation and medical costs, without delay. Associated costs for your life-time care must be compiled. It’s important to objectively evaluate your current and future needs resulting from the onset of your injury.
We have been representing spinal cord injury victims since 2003. If you or a loved one has suffered a spinal cord injury, please call us today, province wide at 1-844-LALANDE or local in the Hamilton/GTA at 905-333-8888. Alternatively, if you simply want to touch base, please feel free to email us through our website. Your email is completely confidential and we will try our best to answer any questions you may have.
LALANDE PERSONAL INJURY LAWYERS – HAMILTON OFFICE
1 King Street East, Suite 1705
Hamilton, On L8P 1A4
905-333-8888
It’s very important that you understand this article does not constitute any type of medical advice whatsoever. We are not doctors. If you have a spinal cord injury medical concern please speak to your doctors immediately. We are spinal cord injury experts in the legal field, meaning that our firm obtains the justice and compensation the spinal cord injury victims deserve. This article is an informational piece only and was written with the assistance of Dr. Jackson and with research through Pubmed, The Journal Of Spinal Cord Injury Medicine, Spinal Cord, The International Journal Of Physical Medicine And Rehabilitation, Spinal Cord Injury And Cases, The American College Of OB/GYN’s, And A Disabled Women’s Guide To Pregnancy And Birth.


